Power Your Software Testing with AI and Cloud
Supercharge QA with AI for Faster & Smarter Software Testing

60 Test Case Examples for HealthCare Domain Testing
- Learning Hub
- 60 Test Case Examples for HealthCare Domain Testing
CHAPTERS
- Overview
- Writing Effective Test Cases
- Snowflake Test Case Template
- CI CD Test Case Template
- Jenkins Test Case Template
- Salesforce Test Case Template
- ServiceNow Test Case Template
- Shopify Test Case Template
- Signup Page Test Case Template
- Ecommerce Test Case Template
- Xamarin Test Case Template
- React Test Case Template
- Angular Test Case Template
- Gaming Platform Test Case Template
- Vercel Test Case Template
- Wix Test Case Template
- CMS Test Case Template
- Flutter Test Case Template
- Site Generator Test Case Template
- Website Builder Test Case Template
- Mobile Development Test Case Template
- Healthcare Domain Test Case Template
- Insurance Domain Test Case Template
- Retail Testing Test Case Template
- Media and Entertainment App Testing Test Case Template
- Telecom Domain Test Case Template
- Travel and Hospitality App Testing Test Case Template
- Test Case Templates For Banking Application Testinge
- Test Cases For The Login And Registration Page
OVERVIEW
Healthcare domain testing evaluates the testing environment for a healthcare application as per criteria like standards, safety, compliance, and interdependence with other organizations. Healthcare domain testing aims to ensure the application's quality, dependability, performance, safety, and efficiency. A thorough testing strategy should be in place because several standards and laws must be adhered to for the software to be used in the healthcare sector.
Healthcare Domain Test Case Examples
Here's a detailed list of Healthcare Domain Test Cases that is accessible to everyone. Please feel free to add suggesstions.
SEE MORE →- Business Process in HealthCare System
- Useful tips for Healthcare Testing
- Testing Types for Healthcare Applications
- Testing of providers system
- Testing of Broker System
- Testing of Member System
- Testing of Claims System
- Testing of Finance System
- Testing for regulatory compliance
- Healthcare Domain Testing with LambdaTest
- Frequently Asked Questions (FAQs)
Business Process in HealthCare System
In the healthcare system, several business processes can benefit from healthcare domain testing. Here are some key business processes:
- Patient registration: Collect patient information when they first visit a healthcare provider. Healthcare domain testing can verify that patient data is correctly captured and stored in the healthcare system.
- Schedule Appointments: Appointment scheduling involves scheduling patient visits with healthcare providers. Healthcare domain testing can ensure that appointments are scheduled correctly and that notifications are sent to patients and providers as needed.
- Medical billing and coding: Medical billing and coding translates medical procedures and diagnoses into codes that can be used for insurance claims and reimbursements. Healthcare domain testing ensures billing and coding are accurate and compliant with healthcare regulations.
- Electronic health record (EHR) management: EHRs manage patient data, including medical histories, diagnoses, and treatments. Healthcare domain testing can verify that EHRs are secure, accurate, and accessible to authorized users.
- Medication management: Medication management involves prescribing, dispensing, and administering medication to patients. Healthcare domain testing can verify that medication is prescribed correctly and dispensed accurately and patients receive the correct dosage.
- Medical device management: Medical devices like monitors and imaging equipment are essential for diagnosing and treating medical conditions. Healthcare domain testing can ensure that medical devices function correctly and that patient data is accurately recorded.
- Telemedicine: Telemedicine involves using technology to provide medical care remotely. Healthcare domain testing can verify that telemedicine platforms are secure, easy to use and provide high-quality care to patients.
Overall, healthcare domain testing can help ensure that healthcare business processes are efficient, accurate, and compliant with healthcare regulations.
Useful tips for Healthcare Testing
Here are some useful tips for healthcare Domain testing:
- Understand the healthcare domain: Healthcare Domain testing requires a deep understanding of the healthcare industry and its regulations and the functional requirements of healthcare software applications. Make sure to research and stay up-to-date on the latest healthcare regulations and best practices for testing in the healthcare industry.
- Test for security and compliance: Healthcare software must comply with various regulations and standards, such as HIPAA, FDA, and Meaningful Use. Test security and compliance by performing security testing, such as penetration testing and vulnerability scanning, as well as regulatory compliance testing.
- Test for accuracy and data quality: Healthcare software must provide accurate results and information. It enables accuracy in data quality by performing functional testing, data validation, data integrity testing, and data consistency testing.
- Test for usability: Healthcare software must be user-friendly, as healthcare professionals and patients rely on these applications to manage healthcare information. Test for usability by performing usability testing and gathering user feedback through Healthcare Domain testing.
- Test for performance and scalability: Healthcare software must perform well, even under heavy loads. Healthcare Domain testing helps improve the performance and scalability of tests by performing load, stress, and scalability testing.
- Test for integration: Healthcare software often must integrate with other systems, such as laboratory systems, medical devices, and billing systems. Test for integration by performing integration testing and verifying that the software can integrate seamlessly with other systems through Healthcare Domain testing.
- Collaborate with healthcare professionals: Healthcare domain testing helps improve the collaboration between software testers and healthcare professionals. Healthcare professionals can provide valuable feedback on the functionality and usability of the software, while software testers can ensure that the software meets the requirements of the healthcare industry.
Overall, healthcare domain testing requires specialized knowledge of the healthcare industry and its regulations and expertise in software testing. By following these tips, software testers can ensure that healthcare software applications are accurate, secure, and user-friendly.

Testing Types for Healthcare Applications
Healthcare applications are complex systems that require rigorous testing to ensure that they meet the needs of their users, including providers, brokers, members, and other stakeholders. To achieve this, several testing types are employed to test different aspects of the application. Let’s discuss the sample test cases for each testing type of Healthcare Domain Testing:
Testing of providers system
Testing of providers system involves verifying that the system used by healthcare providers, such as hospitals, clinics, and physician offices, meets the necessary standards for functionality, security, and compliance. Testing providers systems help ensure that healthcare providers can provide high-quality patient care while maintaining efficient and secure operations.
- Verify that the provider system allows healthcare providers to create a new patient record with all necessary demographic data and contact information.
- Verify that the provider system allows healthcare providers to add and manage clinical notes for each patient and that authorized providers can access and update these notes.
- Verify that the provider system allows healthcare providers to update patient information such as an address, phone number, and insurance information.
- Verify that the provider system can accurately capture and store diagnosis and procedure codes for each patient encounter.
- Verify that the provider system allows healthcare providers to prescribe medications and transmit these prescriptions to pharmacies electronically.
- Verify that the provider system can generate and print patient encounter summaries, clinical notes, and other medical records as needed.
- Verify that the provider system allows healthcare providers to order lab tests and imaging studies and that the results are accurately captured and recorded in the patient record.
- Verify that the provider system can send and receive messages to other healthcare providers, including secure messaging for sensitive patient information.
- Verify that the provider system can create and manage schedules for patient appointments and that authorized providers can access these schedules.
- Verify that the provider system can generate reports on patient visits, diagnoses, and other key metrics for compliance, quality improvement, and other purposes.
- Verify that the broker system allows brokers to create a new user account with all necessary demographic data and contact information.
- Verify that the broker system allows brokers to search and filter available healthcare plans based on different criteria, such as location, benefits, and costs.
- Verify that the broker system allows brokers to compare healthcare plans and generate reports on critical differences.
- Verify that the broker system allows brokers to enroll clients in healthcare plans and that the enrollment process is accurate and complete.
- Verify that the broker system can generate and print client summaries and enrollment confirmations as needed.
- Verify that the broker system allows brokers to manage client accounts, including adding and updating demographic and insurance information.
- Verify that the broker system can accurately capture and store eligibility and enrollment data for each client.
- Verify that the broker system can generate reports on client enrollment, plan utilization, and other vital metrics as needed.
- Verify that the broker system allows brokers to send and receive messages to clients and other stakeholders, including secure messaging for sensitive information.
- Verify that the broker system can support multiple brokers and clients simultaneously without impacting system performance.
- Verify that the member system allows members to create a new account with all necessary demographic data and contact information.
- Verify that the member system allows members to view their healthcare plan benefits, including coverage, deductibles, and copays.
- Verify that the member system allows members to search for healthcare providers and facilities within their plan network.
- Verify that the member system allows members to schedule appointments with healthcare providers and facilities.
- Verify that the member system allows members to access their medical records, including lab results, imaging studies, and clinical notes.
- Verify that the member system allows members to request prescription refills and view their medication history.
- Verify that the member system can generate and print Explanation of Benefits (EOB) statements and other financial records as needed.
- Verify that the member system can accurately capture and store claims data for each medical encounter.
- Verify that the member system allows members to send and receive messages to healthcare providers, including secure messaging for sensitive information.
- Verify that the member system can support multiple users simultaneously without impacting system performance.
- Verify that the claims system can accurately process claims submitted by healthcare providers, including claims for medical services, prescriptions, and medical equipment.
- Verify that the claims system can accurately determine each claim's eligible benefits and copayments.
- Verify that the claims system can accurately adjudicate claims based on the member's coverage and policy rules.
- Verify that the claims system can handle different claims, such as inpatient, outpatient, emergency, and pharmacy.
- Verify that the claims system can accurately identify duplicate and potentially fraudulent claims.
- Verify that the claims system can accurately process claims for multiple procedures and services on a single claim.
- Verify that the claims system can handle claim adjustments and resubmissions as needed.
- Verify that the claims system can generate and send Explanation of Benefits (EOB) statements and other financial records to members and healthcare providers.
- Verify that the claims system can support claim appeals and disputes, including tracking and updating appeals status.
- Verify that the claims system can accurately capture and store claims data for reporting and analytics purposes.
- Verify that the finance system can track and manage member premiums and other financial transactions accurately.
- Verify that the finance system can accurately calculate and apply co-payments, deductibles, and other financial policies.
- Verify that the finance system can handle different payment methods, including credit/debit cards, electronic checks, and bank transfers.
- Verify that the finance system can accurately generate and send member invoices and statements.
- Verify that the finance system can support electronic funds transfer (EFT) and other payment automation features.
- Verify that the finance system can handle different currency and exchange rate scenarios accurately.
- Verify that the finance system can handle payment discrepancies and billing disputes.
- Verify that the finance system can accurately manage accounts receivable and accounts payable.
- Verify that the finance system can generate and send financial reports and analytics, including revenue, profit, and loss statements.
- Verify that the finance system can handle budgeting, forecasting, and financial planning scenarios.
- Verify that the system complies with HIPAA regulations for patient privacy and security.
- Verify that the system complies with the Health Information Technology for Economic and Clinical Health (HITECH) Act.
- Verify that the system accurately tracks and manages drug inventory in compliance with FDA regulations.
- Verify that the system complies with the Affordable Care Act (ACA) regulations for healthcare coverage.
- Verify that the system accurately captures and reports quality measures in compliance with the Centers for Medicare & Medicaid Services (CMS) regulations.
- Verify that the system complies with the Electronic Prescribing of Controlled Substances (EPCS) regulations.
- Verify that the system complies with the Joint Commission standards for healthcare accreditation.
- Verify that the system complies with the Occupational Safety and Health Administration (OSHA) regulations for employee safety.
- Verify that the system complies with the Americans with Disabilities Act (ADA) regulations for accessibility.
- Verify that the system complies with the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) coding standards.
This test case is essential for ensuring the provider system's quality and accuracy and enabling healthcare providers to provide efficient and effective patient care. The test case involves entering patient information, verifying data accuracy, and ensuring the information is correctly saved and displayed in the patient records list.
This feature is critical to patient care, as clinical notes contain important information about a patient's medical history, diagnosis, and treatment plan. The test case involves adding new clinical notes, verifying access and update permissions for authorized providers, and checking that the updated notes are correctly saved and displayed in the patient's record.
This feature is crucial as it ensures that the patient's records are up-to-date and accurate, essential for effective care. The test case involves updating patient information, verifying that the updated information is correctly saved and displayed, and ensuring that any relevant system integrations, such as billing or insurance, are updated with the new information.
This feature is critical to ensure accurate billing, reimbursement, and reporting for patient encounters. The test case involves creating a patient encounter, entering the appropriate codes for diagnosis and procedures, verifying that the codes are accurately captured and stored, and ensuring that any relevant system integrations, such as billing or insurance, are updated with the correct codes.
This feature is critical to ensure accurate and efficient medication management, reduce errors, and improve patient safety. The test case involves creating a medication prescription, verifying that it is correctly transmitted to the pharmacy, and ensuring that the pharmacy can receive and fulfill the prescription as intended.
This feature is essential for maintaining accurate records, providing continuity of care, and ensuring compliance with regulations. The test case involves generating a patient encounter summary, clinical notes, or medical records, verifying that they contain accurate and complete information, and ensuring the printed records are legible and formatted appropriately.
This feature ensures accurate diagnosis, treatment, and patient care. The test case involves ordering lab tests or imaging studies, verifying that the orders are correctly entered into the system, and ensuring that the test results are accurately captured and recorded in the patient record.
The system should be able to handle various message types and ensure the confidentiality and integrity of the information exchanged. The test case involves sending and receiving messages between healthcare providers, verifying that the messages are delivered securely, and the information is accurate.
Authorized providers should be able to access the schedules to view their appointments and make necessary changes. The test case involves creating and managing appointment schedules, verifying that appointments can be added, modified, and canceled as needed and that providers can easily access their schedules.
To ensure that the provider system can generate reports on patient visits, diagnoses, and other key metrics, it is important to verify that it can accurately capture and store relevant data. The system should be able to generate reports in a timely and efficient manner, and these reports should be customizable to meet the healthcare organization's specific needs. Additionally, the system should be capable of securely storing and transmitting these reports to authorized users as needed.
Testing of Broker System
Testing of a broker system involves verifying that the system can accurately and securely manage broker information and transactions. The testing of a broker system plays a critical role in ensuring that the organization can manage its broker relationships and maximize its revenue effectively.
This test includes capturing and storing the user's demographic data and contact information, such as name, address, phone number, and email address. The system should also ensure the information is accurate, complete, easily accessed, and updated. Creating user accounts is a critical function of the broker system, as it enables brokers to manage and provide access to healthcare plans and services for their clients.
The test would involve testing various search and filter options available in the system and ensuring that the results displayed are accurate and relevant to the search criteria. The test would also verify that the system displays complete information about each plan, including benefits, costs, and restrictions. This would ensure brokers can make informed decisions while recommending healthcare plans to their clients.
The testing should ensure that brokers can easily find and compare plans based on different criteria, such as benefits and costs, and that the generated reports accurately reflect the critical differences between the plans. Additionally, the testing should verify that the system can handle a large volume of data and that the comparison and report generation features work efficiently and effectively.
The testing should ensure that the system accurately captures all necessary information from the broker and the client, such as personal information, plan selection, and coverage details, and that this information is transmitted correctly to the insurance carrier. It should also ensure that the enrollment process meets all regulatory and compliance requirements.
This verification ensures the broker system can generate and print client summaries and enrollment confirmations whenever required. The confirmation should contain all the necessary information about the healthcare plans that the clients have enrolled in and their respective coverage details. This verification helps ensure that the enrollment process is accurate and complete and that clients can access all the relevant information they need about their healthcare plans.
This process involves ensuring that the system accurately captures and stores client data, allows for easy management of client accounts, and that updates to client information are appropriately reflected in the system. Additionally, the system should provide appropriate security measures to protect the confidentiality and privacy of client information.
The test includes verifying that the system can accurately store client demographic data, insurance information, and other relevant data required for enrollment. Additionally, the system should be able to provide accurate and up-to-date reports on a client's eligibility and enrollment status.
The reports may be used for compliance, quality improvement, or other purposes. The reports should accurately reflect the relevant data and provide a comprehensive view of the client's status and usage of the plans. The broker system should be able to generate these reports efficiently and effectively.
The test ensures that brokers can stay in touch with clients, provide support and assistance as needed, and address any questions or concerns that may arise during the enrollment process or throughout the coverage period.
This verification ensures that the broker system can handle a high volume of concurrent users without experiencing system performance issues. The goal is to ensure that the system is scalable and can accommodate the needs of multiple brokers and clients at the same time.
Testing of Member System
The primary goal of testing the member system is to identify any defects or issues that may impact the user experience or the system's overall performance. Testing helps to ensure that the system is reliable and secure and provides accurate information to members.
The member system should have a feature that allows new members to create their accounts with all required information, such as name, date of birth, contact information, and insurance information. This feature should be user-friendly and easy to navigate for members to provide accurate information. Additionally, the system should ensure that all data is secure and protected.
To verify that the member system allows members to view their healthcare plan benefits, it must be ensured that the system provides a user-friendly interface that enables members to access and navigate their benefits information easily. Members should be able to view their coverage details, deductibles, copays, and other relevant benefit information without any confusion or ambiguity.
The test includes providers such as doctors, specialists, and hospitals. Members should be able to search based on location, specialty, and other criteria to find the providers that best meet their needs. The search results should show providers covered by their plan and provide information about each provider, such as their contact information, specialties, and ratings.
Members should be able to view available appointment times, select a convenient time, and receive confirmation. The system should also allow members to cancel or reschedule appointments as needed.
The system should ensure that the member's personal health information is kept secure and only accessible by authorized individuals. Additionally, the system should allow members to communicate with their healthcare providers through secure messaging or telehealth services.
The system should be able to display accurate and up-to-date information on prescribed drugs and refill status to help members manage their medications effectively.
The EOB statements should provide a detailed summary of the member's healthcare plan benefits, including coverage, deductibles, copays, and any related costs incurred by the member. These statements should be accurate and complete, and the system should be able to generate them promptly to meet the member's needs.
The data includes the date and type of service, healthcare provider, and associated costs. The system should ensure that the claims data is stored securely and can be easily retrieved for billing or other purposes.
It aims to verify that the system can support secure messaging and maintain the confidentiality, integrity, and availability of the messages exchanged between members and providers. The messaging feature should also allow efficient and timely communication between members and providers.
To verify that the member system can support multiple users simultaneously without impacting system performance, it must be tested under various loads to ensure that it can handle concurrent access by many users without slowing down or crashing. This includes testing the system's response time and ability to handle peak loads and testing for any scalability issues that may arise as user numbers increase.
Testing of Claims System
Testing of the claims system involves verifying that the system accurately processes and manages healthcare claims, including claim submissions, adjudication, and payments. Testing also includes verifying that the system can generate Explanation of Benefits (EOB) statements and other financial records for accurately tracking and managing claim data for analytics purposes.
The test includes verifying that the system can accurately capture and store claims data, process claims on time, and issue payments to providers. The verification also involves testing the system's ability to identify and prevent fraudulent or erroneous claims.
The test involves testing the system's algorithms and rules engine to ensure they accurately process claims based on the member's coverage and plan benefits. The verification process may also involve testing the system's ability to handle complex claims, such as coordinating benefits, out-of-network claims, and prior authorizations.
The claims system should be able to accurately process claims submitted by healthcare providers by determining the eligible benefits and copayments for each claim. It should also accurately adjudicate claims based on the member's coverage and policy rules. The system should ensure that claims are processed correctly, without errors or discrepancies.
It should be able to accurately process and adjudicate claims for various medical services and medications. The system should also be able to determine the eligible benefits and copayments for each claim and ensure that claims are adjudicated based on the member's coverage and policy rules.
The system should be able to analyze claims data and identify any suspicious patterns, such as multiple claims for the same service from the same provider, claims for services not covered by the policy, or claims for services not rendered. The system should also be able to flag these claims for further review and investigation.
The test includes verifying that the system can handle complex claims with multiple services and procedures, accurately adjudicate each service, and prevent errors or overpayments. Additionally, it is essential to ensure that the system can process these claims efficiently and without impacting system performance.
If a claim is denied or rejected, the system should be able to process any corrections or additional information and resubmit the claim for processing. Similarly, suppose there are changes to a previously processed claim, such as changes to the billed amount or procedure codes. In that case, the system should be able to handle these adjustments and update the claim accordingly.
The test involves confirming that the system can generate EOB statements with complete and correct information, including details on the member's coverage, the services rendered, and the amounts paid by the plan and the member. The system should also be able to send these records promptly and securely, ensuring that members and providers receive them promptly and that their privacy and confidentiality are maintained.
The testing will include verifying that the system can receive and process claim appeals, updating the appeal status, and communicating the status to the relevant parties involved. The objective is to ensure that the claims system provides a fair and efficient process for resolving disputes and appeals, which includes a clear and transparent communication mechanism.
The test includes ensuring that the system can capture and store all relevant data associated with each claim, including the provider, the service rendered, the date of service, the cost, and other necessary information. The system should also be able to generate reports and perform analytics on this data to help identify trends and areas for improvement. This is important to ensure that the system can provide valuable insights into the health plan's performance and help identify opportunities to improve the quality and efficiency of care.
Testing of Finance System
Testing of the finance system involves verifying that the system accurately tracks and manages financial transactions, including member premiums, co-payments, deductibles, and other policies. Ensuring the system complies with regulatory requirements and can handle different currency, and exchange rate scenarios are essential.
To verify that the finance system can accurately track and manage member premiums and other financial transactions, it is necessary to ensure that the system can receive and process payment information from multiple sources, such as member payments, employer contributions, and government subsidies. The system should be able to calculate premium amounts based on the member's coverage and plan rules and handle prorated payments for mid-year enrollments and cancellations.
The finance system should accurately calculate and apply co-payments, deductibles, and other financial policies to ensure members are correctly billed for their healthcare expenses. This helps to prevent financial errors and discrepancies that can impact member satisfaction and overall financial performance.
The system should be able to accurately process and record each payment, including any relevant transaction fees. Additionally, the system should provide appropriate security measures to protect sensitive financial data, such as encryption and secure authentication protocols.
The system should be able to generate invoices and statements based on the member's billing cycle and payment preferences and provide accurate information on the member's account balance and payment history. Additionally, the system should be able to send invoices and statements to members through various channels, such as email, mail, or online portals, and ensure the security of the sensitive financial information included in these documents.
The test comprises verifying that the system can accurately process EFT transactions, generate and manage payment schedules, and handle any errors or exceptions that may occur. The system should also be capable of securely storing and transmitting sensitive financial data, such as bank account and credit card information. Finally, the system should be user-friendly and provide members with clear and concise information about payment options and schedules.
The system should be able to accurately convert and calculate payments in different currencies and handle exchange rate fluctuations and updates. This ensures that all financial transactions are accurately recorded and processed, regardless of the currency used.
The system should be able to handle disputes and inquiries from members and accurately update payment records as needed. The testing should cover scenarios where payments are missed, incorrect, or disputed and ensure that the system can accurately calculate any fees or penalties associated with these scenarios.
The test includes tracking and managing outstanding invoices, payments, and refunds. Accurate management of accounts receivable and accounts payable is essential to maintain the organization's financial health and ensure timely payments and collections.
The system will be tested for its ability to manage accounts receivable and payable, handle payment discrepancies and billing disputes, accurately handle different currency and exchange rate scenarios, support electronic funds transfer (EFT) and other payment automation features, generate and send member invoices and statements, accurately calculate and apply co-payments, deductibles, and other financial policies, accurately track and manage member premiums and other financial transactions.
Verification that the finance system can handle budgeting, forecasting, and financial planning scenarios involve ensuring that the system accurately forecasts future revenue and expenses, allows for setting budgets and tracking actual spending against the budget, and provides insights into financial planning scenarios for the organization. This includes financial modeling, scenario planning, and cash flow management features.
Testing for regulatory compliance
Testing for regulatory compliance ensures that a system adheres to the legal requirements and standards set by regulatory bodies in the healthcare industry. Testing for regulatory compliance is critical in ensuring the system is secure, safe, and legally compliant.
Verifying that the system complies with HIPAA regulations involves ensuring that the system has appropriate technical, administrative, and physical safeguards to protect the confidentiality, integrity, and availability of protected health information (PHI). This includes implementing policies and procedures for access control, data backup and recovery, security incident response, and risk assessment and management.
The system should be designed to prevent breaches, unauthorized access, and theft of personal health information. It should also allow individuals to access their health records and request corrections to inaccurate information. Additionally, the system should comply with reporting requirements in the event of a breach of personal health information.
The verification process should confirm that the system accurately tracks drug information, such as drug names, quantities, expiration dates, and lot numbers. It should also verify that the system can generate reports on drug inventory levels and alert staff when inventory levels are low.
Verifying that the system complies with the Affordable Care Act (ACA) regulations involves ensuring that the system accurately tracks and reports on key metrics related to healthcare coverage, such as eligibility, enrollment, and plan selection. The system must also provide accurate and timely reporting on healthcare costs and premiums, as well as comply with regulations related to pre-existing conditions, essential health benefits, and annual and lifetime limits.
The system should be able to accurately capture and report quality measures, such as patient outcomes, patient safety, clinical quality, and patient experience. These measures should be reported in compliance with the regulations set forth by the Centers for Medicare & Medicaid Services (CMS) to ensure that the healthcare organization is providing high-quality care to patients. This will help the healthcare organization identify improvement areas and make informed decisions about resource allocation.
The test includes ensuring that the system meets the requirements for identity proofing, two-factor authentication, and secure transmission of electronic prescriptions. Additionally, the system must comply with state-specific requirements for EPCS, which can vary.
The Joint Commission is a healthcare accrediting body that sets standards for healthcare organizations in the United States. The commission assesses healthcare organizations based on performance and adherence to specific standards to ensure patients receive high-quality care. Verification that the system complies with the Joint Commission standards for healthcare accreditation involves ensuring that the system adheres to the commission's standards for quality of care, patient safety, infection prevention and control, medication management, and other areas critical to patient care. Compliance with these standards can help ensure patients receive safe and effective care.
The system should provide a safe and healthy work environment, ensure employees receive appropriate training and personal protective equipment and comply with all applicable OSHA standards and regulations. This includes maintaining accurate injury and illness records, conducting regular workplace inspections, and promptly addressing any identified hazards or violations.
Verification that the system complies with the Americans with Disabilities Act (ADA) regulations for accessibility ensures that people with disabilities have equal access to information and functionality provided by the system. This includes features such as support for screen readers, keyboard navigation, and color contrast, among others. Compliance with ADA regulations is essential to ensure that the system is usable by all individuals, regardless of their abilities.
Verification of compliance with the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) coding standards ensures that the system accurately captures and reports medical diagnoses and procedures using standardized codes, facilitating interoperability between healthcare providers and payers. Compliance with these coding standards is essential for accurate billing and reimbursement and tracking healthcare quality measures and outcomes.
Healthcare Domain Test Case Examples
Here's a detailed list of Healthcare Domain Test Cases that is accessible to everyone. Please feel free to add suggesstions.
SEE MORE →Healthcare Domain Testing with LambdaTest
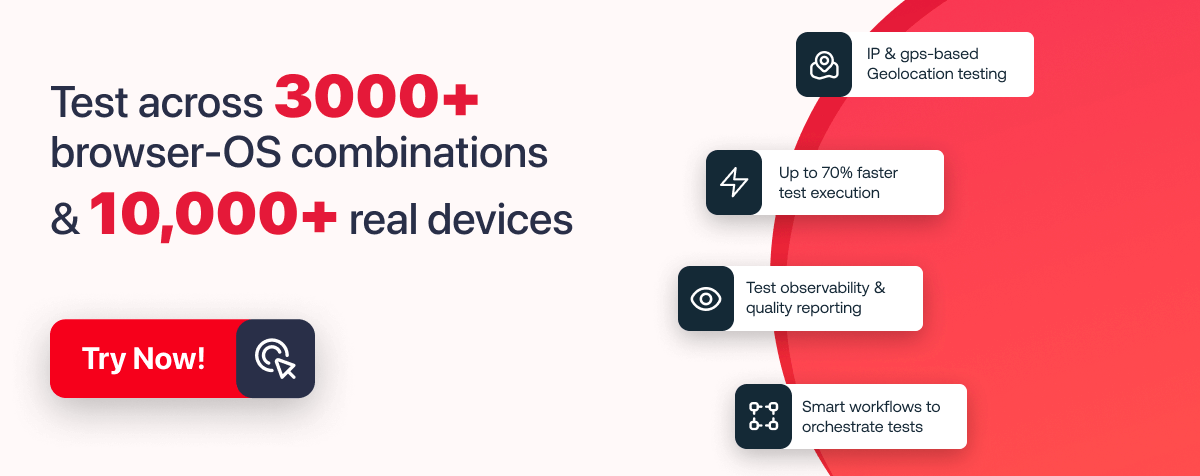
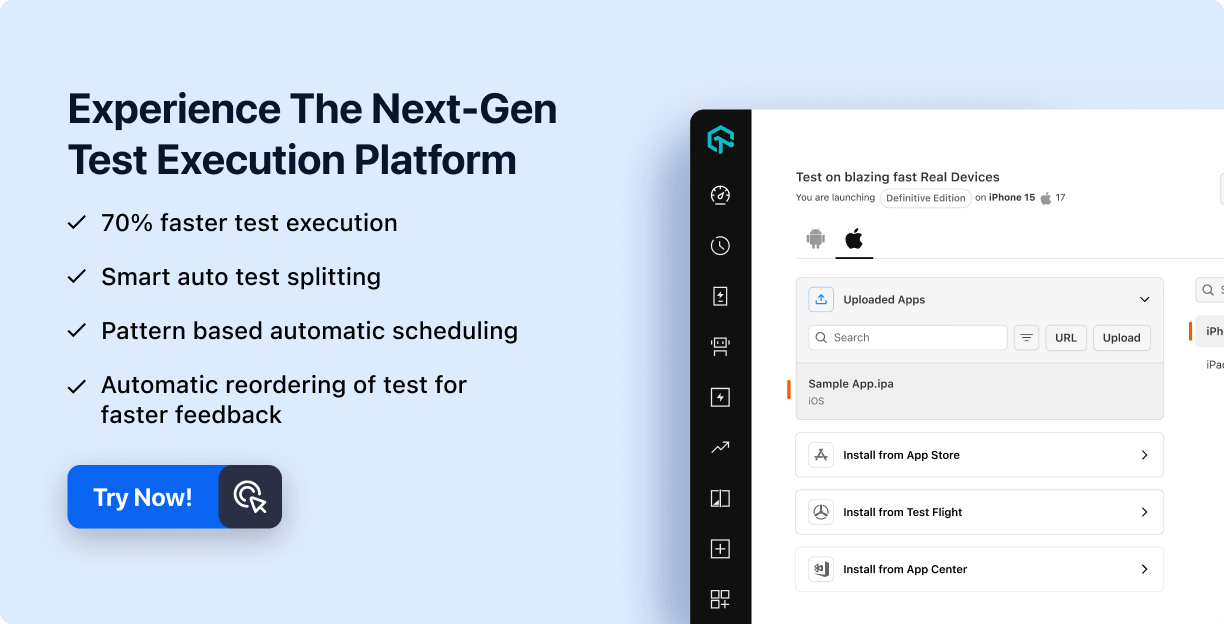
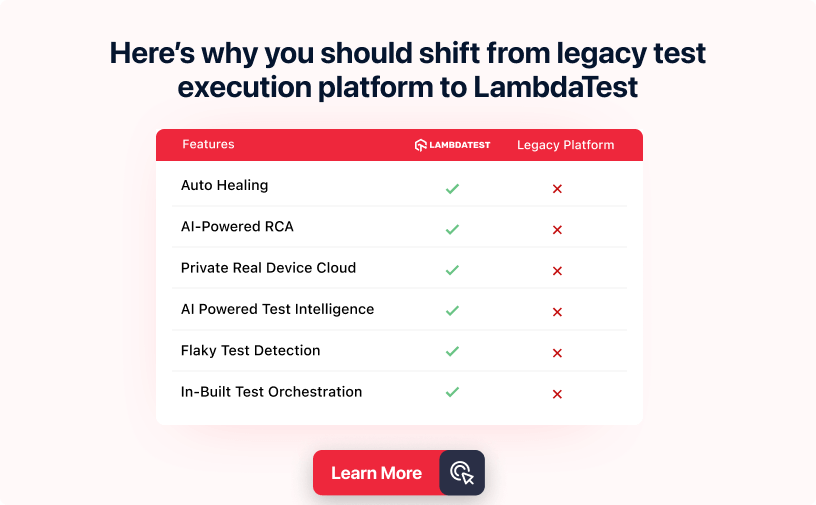
LambdaTest is a cloud-based cross browser testing platform that can help healthcare organizations in several ways when testing their web and mobile applications. Here are some specific examples of how LambdaTest can help in the healthcare domain testing:
- Testing healthcare websites and applications: Healthcare organizations rely heavily on web applications for various purposes, including electronic medical records, patient portals, and telemedicine. LambdaTest allows healthcare organizations to test their web applications on a wide range of browsers, operating systems, and devices to ensure that they function correctly and provide a smooth user experience.
- Cross browser testing: LambdaTest provides cross browser testing capabilities, essential for healthcare organizations to ensure that their applications are accessible to all users, regardless of their browser. Cross browser testing can help healthcare organizations identify and resolve any compatibility issues that may be present in their applications.
- Mobile testing: Healthcare organizations increasingly use mobile applications to deliver healthcare services. LambdaTest provides mobile testing capabilities, allowing organizations to test their mobile applications on various devices and operating systems. It can help healthcare organizations ensure that their mobile applications function correctly and provide a seamless user experience.
- Test automation: LambdaTest provides test automation capabilities that can help healthcare organizations save time and reduce the risk of errors by automating repetitive tests. Test automation can help healthcare organizations ensure that their applications function correctly and provide a high-quality user experience.
LambdaTest can help healthcare organizations ensure the quality and reliability of their web and mobile applications, which is essential for delivering high-quality healthcare services to patients. Aside from HealthCare, LambdaTest supports all major domains such as retail, finance, Insurance, and many others.
Wrapping Up!
Healthcare domain testing is critical to ensuring the quality and safety of healthcare software applications. Given the complex nature of the healthcare industry and the sensitive nature of patient data, it is essential to have a comprehensive testing strategy.
Some of the best practices for healthcare domain testing include developing a clear and detailed test case template, using appropriate testing techniques and tools, leveraging automation, collaborating with subject matter experts, and conducting rigorous testing of scenarios and use cases. By following these best practices and constantly improving their testing processes, healthcare domain testing ensures that software applications meet the highest quality, compliance, and reliability standards while providing patients the best possible care and services.
Frequently Asked Questions (FAQs)
What are the challenges of healthcare domain testing?
Some of the challenges of healthcare domain testing include the complexity of the healthcare industry, the sensitivity of patient data, the need to comply with various regulations and standards, and the diversity of stakeholders and use cases.
What are some commonly used testing techniques in healthcare domain testing?
Some commonly used testing techniques in healthcare domain testing include functional testing, regression testing, performance testing, security testing, and usability testing.
What are the benefits of healthcare domain testing?
The benefits of healthcare domain testing include improved software quality and safety, enhanced patient experience, increased efficiency and productivity, better compliance with regulations and standards, and reduced risks of adverse events and liabilities.
What are some best practices for healthcare domain testing?
Some best practices for healthcare domain testing include developing a clear and detailed testing plan, using appropriate testing techniques and tools, leveraging automation, collaborating with subject matter experts, and conducting rigorous testing of different scenarios and use cases.

Start your journey with LambdaTest
Get 100 minutes of automation test minutes FREE!!
Did you find this page helpful?